Perspectives
Health Equity For All: How Digital Health Can Revolutionize Care for Underserved Healthcare Consumers
 For too long, our nation has grappled with a healthcare system that has marginalized and underserved many communities and populations across the country. Unfortunately, we need not look too far in the annals of history when in search of such accounts. Over the past two years, the country has been witness to the disparate and deleterious impacts that the COVID-19 pandemic has brought upon many Americans. The pandemic has placed a harsh light on what many public health officials and organizations have observed for decades – health inequities can be lethal.
For too long, our nation has grappled with a healthcare system that has marginalized and underserved many communities and populations across the country. Unfortunately, we need not look too far in the annals of history when in search of such accounts. Over the past two years, the country has been witness to the disparate and deleterious impacts that the COVID-19 pandemic has brought upon many Americans. The pandemic has placed a harsh light on what many public health officials and organizations have observed for decades – health inequities can be lethal.
Despite boasting a $20 trillion GDP and spending over $4 trillion on our nation’s health, the US faces stark health disparities, creating a massive financial toll for the country’s health system and its citizens. Annually, the country incurs $135B in direct and indirect costs associated with racial and ethnic health disparities. However, the consequences transcend the financial impact. Health disparities contribute to poor, if not dire, health outcomes for many communities. Black communities are some of the hardest hit populations; Black women face a maternal mortality rate that is 3X greater than is expected for white women, Black men are 70% more likely to die prematurely from stroke, and Black children have a 500% higher death rate from asthma compared with white children. Equally staggering statistics can be found when reviewing the health experiences of low-income Americans, members of the LGBTQIA+ community, as well as rural communities, in addition to other socially and culturally diverse populations. Clearly, many dimensions of health disparity exist throughout the US.
While there are several drivers of inequity, deeply ingrained attitudinal barriers such as mistrust in the nation’s healthcare system and systemic structures, policies, and practices perniciously fuel access gaps and disparities in outcomes. However, a growing body of research and focus on addressing the underlying causes of inequities has brought much-needed light to the social determinants of health (SDOH), including nutrition, housing, transportation, social services, education, employment, and the environment. To this end, local, state, and federal governments have taken measures to address unmet non-clinical SDOH which drive 50% of health outcomes. Though these efforts represent admirable steps in a positive direction, addressing deeply rooted health disparities requires fundamental changes to healthcare delivery.
At 7wireVentures, we believe that this unmet need presents a clear path for digital health companies. In particular, the shift to a digitized healthcare experience opens the door for greater access, increased personalization, and more culturally empathetic care experiences. However, digital health companies cannot address health equity challenges alone. Achieving health equity requires multifaceted and collaborative cross-sector approaches. Those seeking to make the largest impact can partner with key stakeholders including state governments, NGOs, employers, providers, and payers to expand their reach and increase the affordability of care. Ultimately, digital health is poised to play a vital role in achieving what should be the core objective of our health system: Equitable outcomes for all Americans.
Health Equity Landscape
The past two years has experienced massive private investment in the health equity market, reaching nearly $4B in 20211. Recent growth has largely been driven by later stage companies raising mega rounds, such as Cityblock’s $192M Series C extension and $400M Series D round.
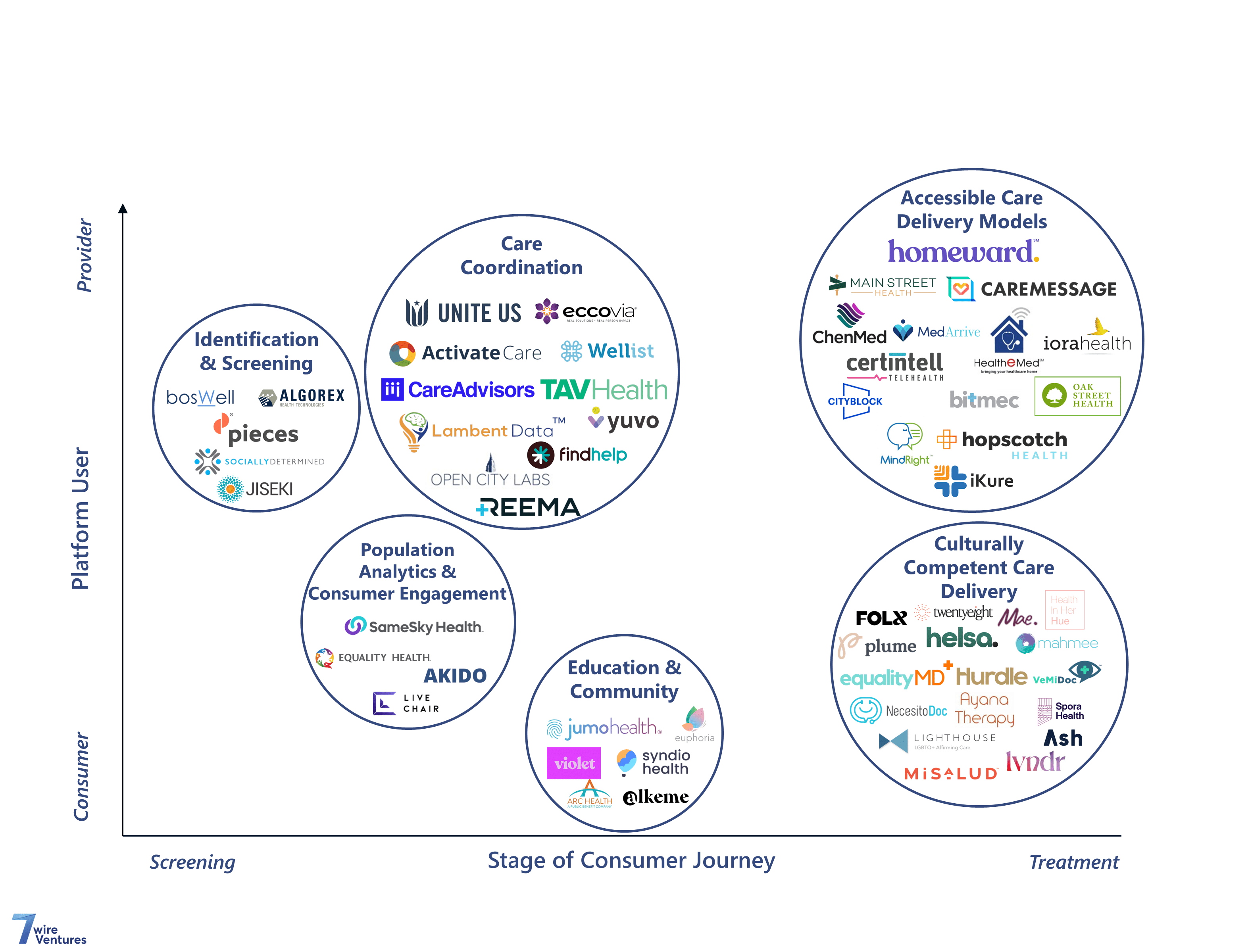
At 7wireVentures, we view the rapidly growing health equity market through the lens of six primary verticals: Population Analytics & Consumer Engagement, Culturally Competent Care Delivery, Accessible Care Delivery Models, Education & Community, Care Coordination, and Identification & Screening.
[1] Pitchbook
Digital Solutions for Health Equity Market Map
 Population Analytics & Consumer Engagement: Advanced population data analytics can enable healthcare organizations to eliminate care gaps, improve care delivery, and provide culturally appropriate engagement for vulnerable populations. 7wireVentures portfolio company SameSky Health‘s multicultural engagement platform guides health plan members and patients on their care journeys by building trusted relationships as they navigate the healthcare system. Other companies like, Live Chair Health, reduce care disparities and attitudinal barriers by meeting consumers in the settings they trust the most, including barbershops, hair salons, and churches where the company offers health screenings, resources, and critical education for chronic conditions.
Population Analytics & Consumer Engagement: Advanced population data analytics can enable healthcare organizations to eliminate care gaps, improve care delivery, and provide culturally appropriate engagement for vulnerable populations. 7wireVentures portfolio company SameSky Health‘s multicultural engagement platform guides health plan members and patients on their care journeys by building trusted relationships as they navigate the healthcare system. Other companies like, Live Chair Health, reduce care disparities and attitudinal barriers by meeting consumers in the settings they trust the most, including barbershops, hair salons, and churches where the company offers health screenings, resources, and critical education for chronic conditions.
Culturally Competent Care Delivery: As the nation grows increasingly diverse, there is a growing disconnect between the backgrounds of healthcare providers and those of the populations they treat. As of 2018, 56% of the US physician workforce was white yet the combined minority population is projected to become the majority by 2042. Additionally, 80% of non-English speaking home care patients are not visited by providers who speak their language.
However, awareness of the impact that social, cultural, and linguistic factors can have on health outcomes is becoming increasingly pervasive. Consequently, we have witnessed a rise in the number of companies focused on delivering healthcare services that improve access to culturally sensitive providers and approaches to health engagement. These specialized digital solutions deliver tailored care for vulnerable populations by curating and deploying highly trained provider networks that are well-versed in the communities they serve. For example, FOLX Health leverages a diverse network of queer and trans specialized providers to deliver end-to-end virtual primary care, HRT, PrEP, and care navigation to help address the many challenges the LGBTQIA+ community faces when interacting with the health system. Similarly, Hurdle, a virtual mental health provider, uniquely specializes in providing convenient access to tailored care and content for people of color, ultimately expanding behavioral care access for underserved populations through non-stigmatizing and culturally sensitive support.
In a country where one’s lived experiences and hardships are uniquely tied to their contextual backgrounds; culturally competent care delivery serves as the cornerstone of improved population health.
Accessible Care Delivery Models: Each community encounters different challenges when attempting to access much needed care. MedArrive, a 7wireVentures portfolio company, provides a care management platform that enables healthcare providers and payers to extend services into the home through a network of EMS professionals. The company supports underserved populations in overcoming healthcare barriers by meeting them where they are and coordinating care with the clinicians they trust. Similarly, Homeward delivers a hybrid virtual and in-person model of care for aging rural communities in need of primary and specialty care services. To accommodate the specific needs of rural communities, the company’s telehealth and remote monitoring services rely on cellular network connections instead of broadband internet given the limited access to high-speed internet that some rural counties experience. Further, the company’s in-person care services are delivered through mobile units that can be accessed by members in central community-based locations, such as church or library parking lots.
Education & Community: Some underserved groups must take it upon themselves to seek out health information relevant to their needs and community. LGBTQIA+ youth, for example, are 5x more likely to look online for information pertaining to their sexuality and health compared to non-LGBTQIA+ youth. Furthermore, many health consumers look online in search of empathetic communities that mirror their own lived experiences. In fact, 92% of patients say online health communities play an important role in their healthcare decisions. As a result, some companies are focused on developing non-stigmatizing, culturally sensitive, and population-specific educational content and social networks. Alkeme, for example, offers therapist-led wellbeing courses, guided meditations, and audio therapies with a focus on the Black experience. Violet, on the other hand, benchmarks and publicly recognizes the cultural competence of clinicians and care team members, allowing consumers to easily find the right provider for them. Further, the company provides continuing cultural competency training and education to upskill providers on delivering inclusive healthcare.
Care Coordination: Coordinated care has become increasingly necessary as the prevalence of chronic conditions continues to grow in the US. This need however becomes further complicated when considering the various SDOH challenges many Americans face. For example, 59% of Medicaid beneficiaries had at least one ER visit in the past year due to difficulty accessing transportation to their PCP. To address these challenges, , new regulatory proposals seek to increase provider accountability for and coordination of SDOH activities. Companies like Unite Us are primed to support these efforts through coordinated care networks of health and social service providers. Dedicated software further helps the company improve coordination, track outcomes, and help standardize data sharing between payers, providers, government services, and social services. Similarly, Reema works with health plans to provide relevant health and social care resources to hard-to-reach members. The company achieves this through a network of local community health workers that are augmented by a data-driven care platform.
Identification & Screening: While there has been a growing focus on addressing the full spectrum of SDOH, due to a lack of financial resources, time, and economic incentives, only 24% of hospitals reported screening for SDOH. Yet there is a clear impact on downstream care. For example, patients with at least 2 unmet SDOH needs are 3X more likely to have a preventable readmission. This disconnect presents a pressing need to efficiently identify high risk patients and determine the various social, economic, and access challenges they may have.
Pieces Technologies interprets patient information in real-time, connecting health systems and community-based organizations to support healthier outcomes both in and out of the hospital. Additionally, Socially Determined provides social risk intelligence solutions to organizations, giving visibility into where and how socioeconomic factors are impacting their members and allowing for highly optimized interventions for some of the most complex populations.
7wireVentures Predictions
PREDICTION 1: As the efficacy of delivering culturally competent care becomes more widely recognized and the country continues to grow increasingly diverse, stakeholders will intentionally build culturally-trained provider networks to meet the unique needs of their members and patients.
Across a variety of underserved populations, we see key unmet needs. For example, 1/3 of Medicaid members are Spanish speakers, reinforcing the necessity to include multilingual and culturally sensitive services. Additionally, 7 out of 10 LGBTQIA+ patients have experienced negative care, causing many to avoid healthcare settings altogether. On the provider side, some reports indicate that as much as 31% of PCPs surveyed do not feel capable of providing routine care to transgender patients. To bridge this gap, providers will seek to create culturally competent and diverse provider networks initially through partnerships and formalized cultural competency training, that can deliver personalized care based on language, race, and sexual orientation. Over time, personalized care will come to mean that consumers can receive care from someone who looks like them, speaks their native language, and deeply understands culturally relevant care preferences. To achieve this, we believe digital health will fuel a wave of consolidation via acquisitions of culturally competent care providers, with the Included Health merger with Grand Rounds and Doctor on Demand paving the path. Long term, traditional providers will follow suit and build diverse provider networks though M&A and strategic partnerships.
PREDICTION 2: Healthcare that meets consumers where they are – including at-home, virtually, or in hybrid models, will become a core strategy for closing care gaps for hard-to-reach populations including Medicaid, dual-eligible members, and more broadly rural populations located in healthcare deserts.
The pandemic prompted the acceleration of care at home, in part due to the proven capabilities of telehealth. New care delivery organizations have emerged offering hybrid models of virtual and in-person care centered around the home and are demonstrating value with vulnerable and hard-to-reach populations. To accelerate the advent of new home-centric clinical models, healthcare stakeholders will quickly move to work closer together. We have already seen successful examples of this, such as MedArrive and Molina’s partnership to provide in-home health services for vulnerable and hard-to-reach Medicaid members in Texas. Long term, with additional adoption and data, we expect increased investment by health systems to facilitate the delivery of at-home care and to equip vulnerable populations with the necessary technology they need (e.g., Wi-Fi, connected device, iPads) to access care equitably.
PREDICTION 3: Health plans will continue to leverage data-driven personalized communication strategies to activate hard-to-reach members. Over time, as health plans increasingly focus on capturing social determinant data, multicultural patient engagement techniques will become widespread.
Using a one-size-fits-all approach to member outreach has proven to be ineffective. Consequently, health plans are increasingly leveraging multi-modal channels (e.g., text, chat, phone, email) that align with member preferences. In particular, sophisticated health plans will soon leverage data science and behavioral research to create an even more personalized outreach strategy, which will drive engagement and behavior change for difficult-to-reach members.
Long term, as more stakeholders gather cultural and social determinants of health data and observe the outsized impact of multicultural communication, these strategies will become table stakes. For example, 59% of care gaps were closed when leveraging a multicultural patient engagement solution across 7K patients. To date, we’ve seen meaningful partnerships in this space. Blue Shield of California and SameSky Health have partnered to improve Medi-Cal member health outcomes through language appropriate and culturally relevant text-messaging. Ultimately, these changes will help improve member engagement, close care gaps, and drive improved health outcomes.
PREDICTION 4: As social determinants of health interventions are used more frequently in healthcare, standardized approaches to measuring SDOH data and impact will emerge to drive more precise risk-based payment models and eventually, encourage providers in vulnerable communities to consider value-based payment programs.
Beginning in 2023, the Center for Medicare and Medicaid Innovation (CMMI) will require healthcare organizations participating in new value-based payment models to create health equity plans. As a result, healthcare organizations are working to identify specific social needs by collecting non-medical, demographic data. To meet this need at scale, we expect to see increased partnerships across healthcare technology platforms, enabling a shift towards standardized SDOH data. Many such efforts are already underway, including Lyft Health’s integration with Epic and Cerner’s partnership with Jvion. Ultimately, we expect healthcare organizations to use these rich datasets of non-medical information to design interventions with the primary goal of closing equity gaps. Further, we expect to increasingly see health stakeholders implement technology solutions that coordinate care and predict risk tied to social determinants of health on an individual level.
Despite growing awareness of health disparities and encouraging progress made in increasing health equity, there is still much work to be done. In close collaboration with cross-sector partners, digital health presents a catalyzing opportunity to close dire health equity gaps that have plagued many of the nation’s communities for far too long. Through thoughtful consumer-centric design and application, these innovative solutions and partnerships have the potential to reimagine the care experience for historically marginalized and underserved populations, and ultimately engender a nation of Informed Connected Health Consumers who are well equipped to achieve equitable health and wellbeing.